
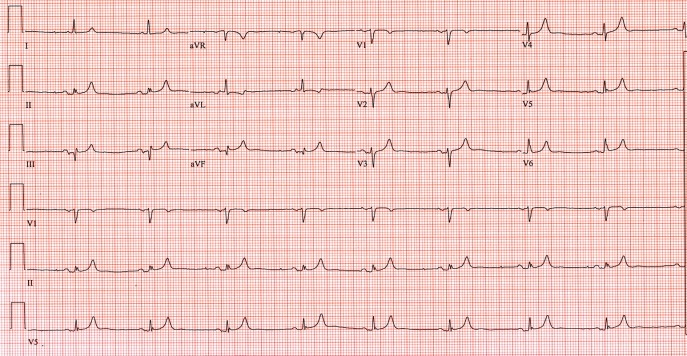
Mild-to-moderate hyperkalemia causes depression of conduction between adjacent cardiac myocytes, resulting in the prolongation of the PR and QRS intervals as potassium levels increase. The effect of hyperkalemia depends on the tissue involved, with the atrial myocardium being the most sensitive, the ventricular myocardium less sensitive, and the specialized tissue (sinoatrial node and His bundle) the least sensitive. Hyperkalemia decreases the resting membrane potential (RMP), the magnitude of the action potential, and the maximum rate of increase of phase 0 in the cardiac muscle. A high concentration of extracellular potassium slows impulse conduction through all cardiac tissue, accounting for numerous EKG findings. These EKG changes can be explained by the physiological effect of potassium on myocardial cells. Sequential EKG changes noted with rising potassium levels include peaked T-waves, prolonged PR interval, prolonged QRS, loss of P-wave, escape rhythms, sine wave configuration, ventricular fibrillation, and pulseless activity or asystole. However, EKG findings in hyperkalemia are seen in only 50-64% of patients with potassium levels of more than 6.5 mEq/L. Hyperkalemia may be associated with EKG changes. Although new-onset LBBB could have been due to myocardial infarction/ischemia or hyperkalemia, due to a history of ESRD with missed hemodialysis, we treated this as a case of severe hyperkalemia which was confirmed with serum potassium level. On review of records, a normal baseline EKG with no structural heart disease was noted. Her initial EKG showed a heart rate of 92 beats per minute, PR interval of 222 ms, QRS duration of 174 ms, dominant S-wave in V1, broad monophasic R-wave in lateral leads, absence of Q-wave in lateral leads (I, aVL, V5-V6), and left axis deviation, suggestive of LBBB (Figure (Figure1). The laboratory analysis showed severe hyperkalemia with a serum potassium level of 8.5 mEq/L, blood urea nitrogen of 118 mg/dL, creatinine of 13 mg/dL, sodium of 134 mEq/L, chloride of 99 mEq/L, bicarbonate of 22 mmol/L, and calcium of 9.4 mg/dL. General and systemic examinations were suggestive of volume overload.

On arrival to the ED, her heart rate was 110 beats per minute, blood pressure was 210/90 mmHg, respiratory rate was 22 breaths per minute, and oxygen saturation was 90% on 2 L of oxygen.

A 48-year-old female with ESRD on hemodialysis presented to the emergency department (ED) with complaints of generalized weakness and shortness of breath after she missed one hemodialysis session.


 0 kommentar(er)
0 kommentar(er)
